A 60 year old male with chief complaints of abdominal pain and distesioy
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
A 60 year old male resident of kodad labourer by occupation came with chief complaints of abdominal swelling since 3 months and abdominal pain since 3 months
History of presenting illness: patient was apparently asymptomatic untill 3 months ago then then he developed abdominal distension which was sudden in onset gradually progressive associated with sob grade 3 according to MMRC scale as swelling progressed, no aggravating factors ascitic tap was done twice in a local hospital in nakgonda and the fluid was about 750 ml which made the distension decreased temporarily.
He also complained of pain in abdomen which started in right hypochondium and then beacame diffuse sudden dragging type no aggravating or relieving factor no radiating.
He also complained of loss of appetite
No h/o vomiting
No h/o dysphagia
No h/o melaena
No h/o hemetemesis
No h/o constipation
No h/o melaena
No h/o heart burn
No h/o steatorrhea
No h/o cough,cold,PND, Sweating, palpitations
Past history: he had jaundice 2 years ago he uses herbal medicine.
Not a k/c/o HTN, asthma, epilepsy,Dm,TB.
History of ascitic tap done
Family history: no significance
Personal history:
Diet: mixed
Appetite: decreased
Sleep: inadequate since 3 months
bladder: regular
Bowel: regular
Alchol addictions for 25 years he drank about 120 ml of whiskey
No tobacco addictions
No allergies
General examination : patient was conscious coherent cooperative and was moderately built and nourished
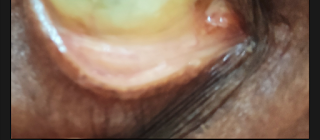
Pallor: present
Icterus: absent
Cyanosis: absent
Clubbing: absent
Lymphadenopathy:absent
Edema: absent
Vitals:
Temperature - afebrile
PR :- 88bpm
BP :- 130/80 mm Hg
RR:- 20cpm
Systemic examination:
Abdomen examination
Shape of the abdomen: distended
No scars,No engorged veins
Umbilicus at the level of abdomen
Hernial orifices: normal
Flanks are full
Palpation:
Superficial palpation:
No local rise of temperature
No tenderness
Deep palpable :
No palpable mass
Liver not palpated
Spleen not palpated
Kidney not palpated
Abdominal girth:
Inspiratiory:87cms
Expiratory:82 cms
Percussion:
Shifting dullness present
Fluid thrill absent
Liver span-12 cms
Auscultation: bowel sounds heard
CVS:thrills: No
S1,S2 heard,no murmurs
Respiratory system:
Trachea: Central
Breadth sounds: heard
No additional sounds
Provisional diagnosis:
Ascites secondary to chronic liver disease
Investigations:
Treatment:
FLUID RESTRICTION 1.5L day
Salt restriction less than 2grams/day
TAB. ALDACTONE 50mg per oral OD
Tab lasix 20mg per oral BD
Protein powder 2 scoops in a glass of milk per oral BD
Daily abdominal girth monitoring
Vital monitoring 4th hourly.







Comments
Post a Comment